Drug Management Tools
Drug Management-Tools: Pre-authorizations & Step Therapies

Drug management tools (DMTs) are mechanisms designed to optimize patient outcomes and ensure the most appropriate use of medications, while reducing waste, error, and unnecessary prescription drug use and cost. DMTs are developed by a Pharmacy and Therapeutics (P&T) committee to promote the use of cost-effective and high-quality prescription medication. The P&T committee is comprised of physicians, pharmacists, medical researchers, and other healthcare experts. Examples of DMTs are Prior Authorizations (PA), Step Therapies (ST), Specialty Limits (SL), Quantity Limits (QL), and Age Limits (AL). The P&T Committee is in charge of determining the appropriate DMT for a drug based on the clinical data, FDA package insert, clinical guidelines, and cost-implications. The implementation of a drug management tool ensures that the patient will receive the more effective and safe treatment, while ensuring the best outcomes.
Prior Authorization
A ‘PA’ or prior authorization is a process that reviews if a treatment plan is medically necessary for the patient. This encourages clinically indicated, safe, and cost-effective medication use by allowing coverage when the prescription is adequate to treat the patient's condition. Treatments that may require a prior authorization usually have the following characteristics:
- Medical treatments that have lower cost and equally effective alternative
- Drugs and therapies that must be used for a specific health condition
- Treatments or medications that are frequently misused
- Medications that are approved only for rare diseases
- Drugs with dangerous side effects or that can be harmful when combined with other medications
- Drugs that require previous use of other treatments or laboratory tests
When your pharmacy is processing a claim for a drug that has a drug management tool, the claim will show a ‘Prior authorization required’ message. The pharmacy will then start the prior authorization process. Usually, medical diagnosis and justification are needed to validate why the treatment is necessary. If clinical criteria is met and the prior-authorization is approved, treatment will be covered. If the pre-authorization is not approved, you and your health care provider may request a reconsideration.
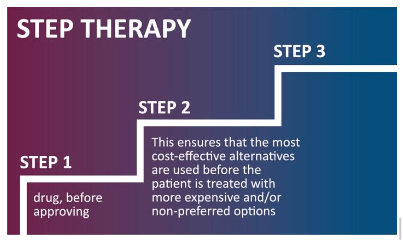
Step Therapy
Step Therapy is a process where a prerequisite drug is required first before the prescribed drug is covered. This ensures that the patient has tried preferred medications with a proven track record that may be better tolerated, less expensive, or less likely to cause interactions. A Step Therapy follows a mechanism where the adjudication system reviews the medication history to determine if the patient has already been treated with the ‘Step 1’ drug, before approving ‘Step 2’ drugs. This ensures that the most cost-effective alternatives are used before the patient is treated with more expensive and/or non-preferred options.
Don’t more expensive drugs work better?
A higher cost does not automatically mean a better drug. For example, a brand drug may have a less-expensive bioequivalent, generic, or brand alternative that might be an option. Bioequivalent/generic and brand drugs must meet the same standards set by the U.S. Food and Drug Administration (FDA) for safety and effectiveness. Talk to your provider to determine which medication options are best for you.
Drug Management Tools encourage safe and cost-effective medication use, and also help manage the rising cost of prescription drugs for everyone. They also provide a patient benefit that reduces treatment prescription costs providing low-cost alternatives.
It is recommended that you review your plan benefit documents or call for more information about treatments, services, and supplies that require any DMT under your health plan coverage.